Despite decades of medical progress, women’s health remains chronically under-researched and underfunded, writes Dr Ariella Heffernan-Marks. When women are told that their instincts are wrong, they lose confidence not only in their healthcare providers but in themselves.

When I was in my third year of medical school, I found myself battling chronic migraines so debilitating that I could barely function. As a medical student, I was in the privileged position of understanding these symptoms, knowing something wasn’t right and seeking help. Instead of answers, I was met with dismissal.
“It’s just anxiety,” I was told. My pain, my intuition that something was truly wrong, was trivialised and ignored. That experience was not just a personal setback; it was a revelation. It exposed a persistent crisis in women’s healthcare, one that is costing lives, dignity, and, as recent research shows, over $1 trillion globally each year.
Despite decades of medical progress, women’s health remains chronically under-researched and underfunded. The consequences are severe. Women are more likely to be misdiagnosed, their symptoms dismissed, and their pain minimised. The gender health gap is a reality that affects millions of women every day. Whether it’s endometriosis, heart disease, or autoimmune conditions, women routinely face longer diagnostic delays and poorer health outcomes than men.
This gender health gap is not just a matter of economics or policy. It’s about the stories I hear from women from all ages, each with the same frustration, “I knew something was wrong, but no one listened.”
Intuition is often dismissed as “just a feeling,” especially when it comes from women. But in healthcare, intuition is frequently the first indicator that something isn’t quite right.
Time and time again, I’ve witnessed women who know their bodies best, yet their concerns have fallen on deaf ears if their experience does not reflect a textbook experience. I am in no way saying that doctors are not listening or acting in the best interest of their patients – it’s our entire healthcare system is structured to prioritise data and results over lived experience.
This dismissal is not insignificant. It leads to missed diagnoses, unnecessary pain, and a profound loss of trust in the system. It takes four years on average for women to be diagnosed with a general health condition, and 6 – 9 years for more complex conditions like Endometriosis.

Globally, women spend 25% more time in poor health than men. This is mostly during their working years (aged 20-65), meaning it affects their ability to go to work and therefore access the health services they and their families need.
When women are told that their instincts are wrong, they lose confidence not only in their healthcare providers but in themselves. This slow and constant chipping away of confidence and agency is perhaps one of the most dangerous parts of the gender health gap.
“Technology can support this process and utilise women’s intuition in a data-driven, evidence-based way.”
Dr Ariella Heffernan-Marks
The fragmentation of care further adds to this frustration, as women seek to juggle multiple providers, sources of information, and apps that offer to reduce this burden. There is no single, unified system that tracks a woman’s health across her lifespan if she wishes to do so.
Which led me to question why women don’t have a comprehensive health record. And if one were to exist, how could it include all relevant health data like reports, medications, appointments and also small pieces of information that, when assessed against a bigger picture, add up to something important.
This was the foundation for Ovum – to design the first AI health partner designed specifically for women. More than just an app, it’s a personalised, intuitive, and intelligent health companion.
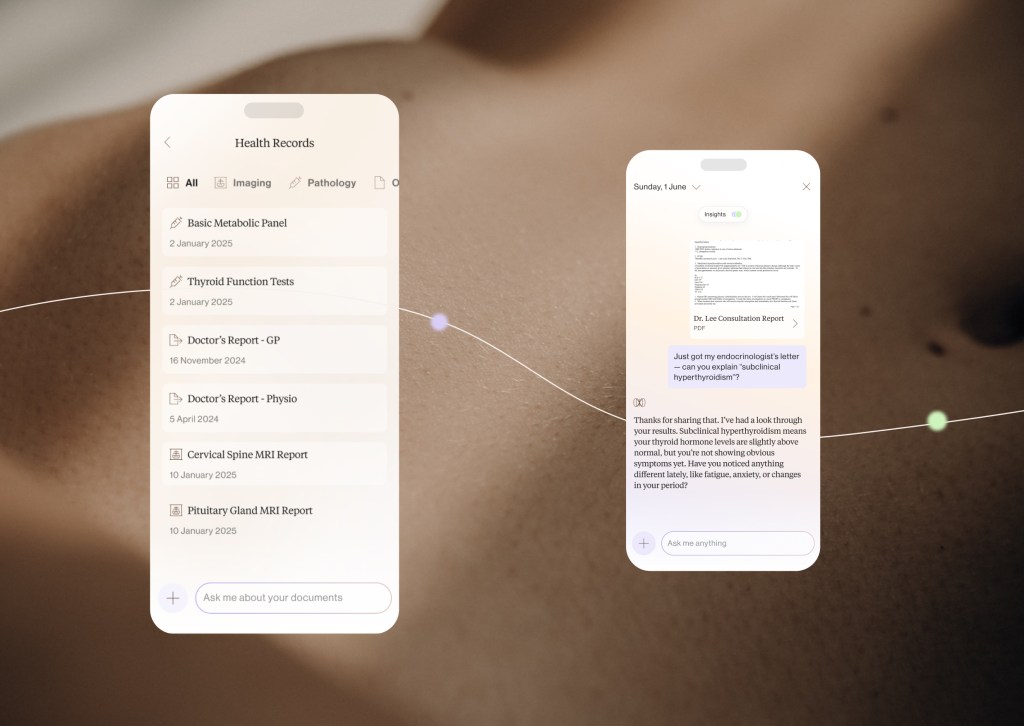
It also creates a longitudinal memory of a woman’s health, offering insights and advice tailored to her unique physiology and life stage. Built by women, for women, Ovum directly addresses the biases that exist in both healthcare and artificial intelligence.
Ovum does not replace doctors or healthcare professionals; it seeks to support them. Importantly, it is an advocate a woman can carry in her pocket into appointments, and use to navigate our healthcare system with data and confidence.
We’ve heard firsthand how empowering and transformative ownership of one’s health data can be. This empowerment is beyond “just a feeling.” In just three years, Ovum has gone from a lightbulb idea to exceeding a $1.7 million pre-seed round, preparing for launch on the app store, and launching clinical trials.
“Every step of this journey was guided by data, research and science, with my secret ingredient being intuition. Our healthcare system and policymakers must listen to women.”
Dr Ariella Heffernan-Marks
Feedback from our Beta testing includes “Ovum learns from my inputs and can provide more detailed feedback based on my daily logging,” and “I can talk to it about anything big or small and it feels like Ovum really cares, will take everything seriously and give info needed to go from there.”
Technology can support this process and utilise women’s intuition in a data-driven, evidence-based way. Investing in women-centred, inclusive technology that bridges the gender health gap and puts women’s voices at the heart of healthcare design is the first step of unlocking the transformational power of technology in women’s healthcare.
We can’t afford to ignore women’s intuition any longer, from a health, economic and moral perspective. When we listen, we all stand to gain.
Dr Ariella Heffernan-Marks is the founder and CEO of Ovum, and a PhD candidate at UNSW and The George Institute.
Look back on the week that was with hand-picked articles from Australia and around the world. Sign up to the Forbes Australia newsletter here or become a member here.