The Royal Flying Doctor Service (RFDS) has launched a nation-wide electronic health record (EHR), bringing a “digital set of extra hands” to clinicians in the sky, in remote areas.

When Oracle’s Red Bull Racing driver Max Verstappen won the Hungarian Grand Prix by nearly eight seconds in July 2022, the world was watching – and so was the RFDS.
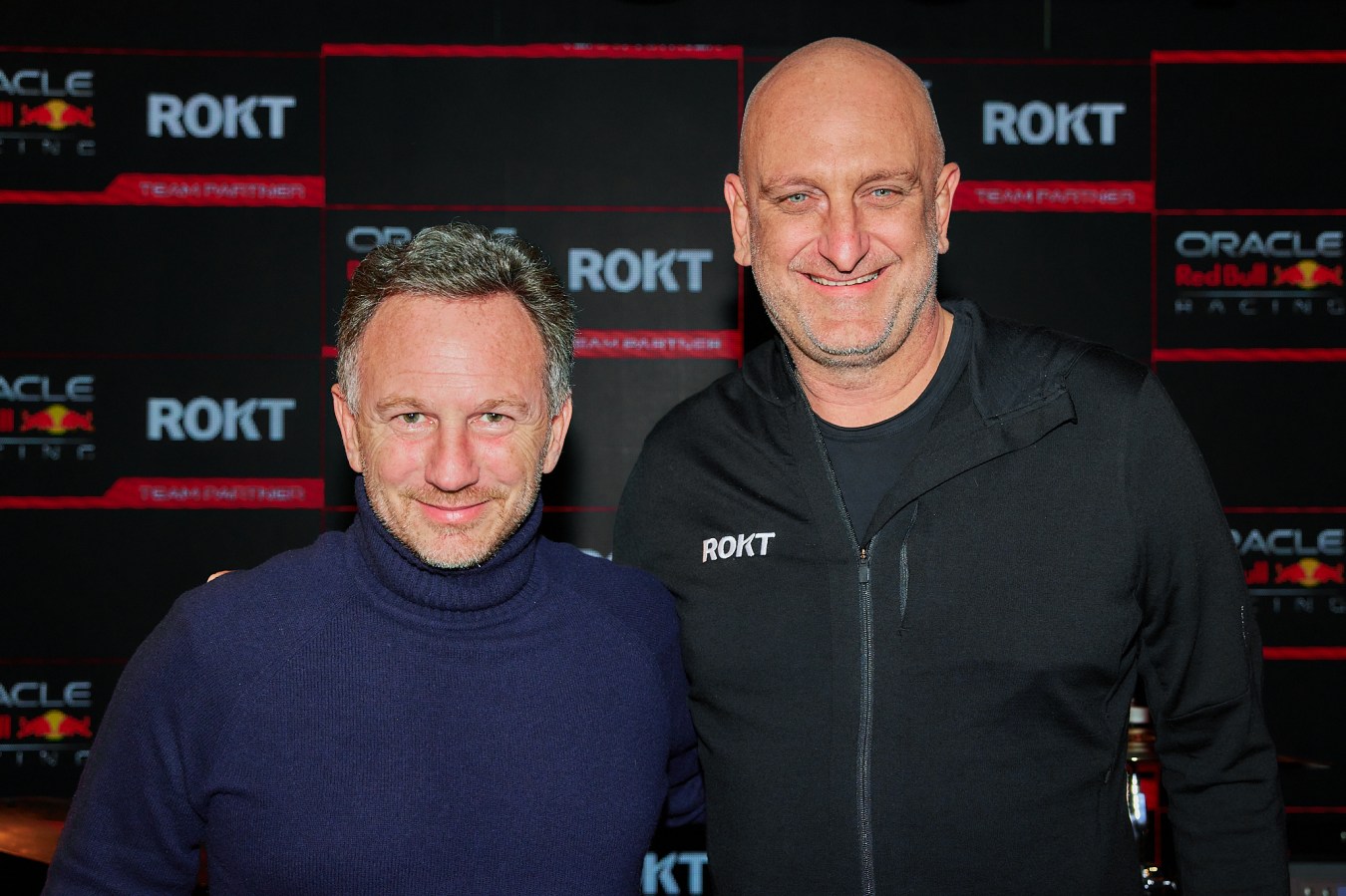
Red Bull’s F1 team had partnered with American tech firm Oracle in early 2021, under a US$300 million sponsorship deal. That partnership didn’t just see Red Bull’s F1 team receive a major a cash injection – it also received a hit of technology capability that would eventuate in Verstappen’s famous win. Today, Oracle Red Bull Racing relies on data simulations they run on Oracle’s Cloud Infrastructure (OCI) to give drivers like Verstappen and Sergio Pérez the best chance to stand on the podium.
“Oracle Red Bull Racing captivated us,” RFDS digital lead, EHR Project, Ryan Klose, says. “What it’s done is, it’s highlighted what data can do from a telemetry and real-time sense. It showcased that data can be real-time now – it doesn’t have to be rest and reused.”
It was this partnership that inspired the RFDS to reform its patient data recording system completely. Today, its electronic health record (EHR) system runs on that same system used by Oracle Red Bull Racing – the OCI. Now, clinicians in the sky can ensure patient and emergency incident data are entered via an App and synchronised automatically out in the field.

“You can have a flight nurse operating the iPad, a doctor on the ground and someone in the operations centre all contributing to the same patient record,” Klose says. “The paper is gone. It used to be an administrative nightmare, which we’ve now overcome.”
This, Klose says, has cut administrative costs by about 20% and data entry staff are being upskilled into more important data management roles.
But the RFDS has built out its solution further – it’s created a digital data twin for an offline mode that allows a live replication of the database. This means even without internet connectivity, clinicians in rural areas can access patient information and update it – and it will sync within seconds of reaching internet connection again.
The ability to work offline is key for the RFDS, which services 7 million people – or 28% of the Australian population – that live in rural and remote areas. Here, internet is not continuous or overly reliable, Klose says, and often clinicians are left at the mercy of their notes and satellite phones to get through.

“Our digital data twin gives us the accuracy and authenticity of data at any time for the patient.”
For clinicians, it’s been a massive move, Dr Mardi Steere, RFDS Clinical Lead, EHR Project, says. “You’re not just dealing with paperwork – you’re dealing with wind, dust, rain, moving transport… There are so many opportunities to lose information, damage information or incompletely communicate information.”
Dr Steere says there’ll also be flags for crew resource management. For example, if a clinician has been on duty for six hours, the app may prompt the user to undergo a handover. “We’ll be able to use that data to build team safety, too.”

The app is also connected into the government’s MyHealth Record system, which is used by hospitals. This means that when the RFDS discharges its patients, the information is pre-loaded into MyHealth for doctors on the ground to work with.
So far, the new EHR is live in South Australia, the Northern Territory and New South Wales, with Queensland set to go live in September. As of today, 7,000 electronic patient episodes have been processed through the new application, with zero outage.
Eventually, the plan is for the EHR to expand its data collection capability to include picking up situational data, health equipment data, environmental data and aviation data. Not only are the administrative benefits clear, Klose says the benefits for the clinicians are clear, too.
Related
“We have future-proofed a little bit for AI here,” Klose says. “What we know is, when a patient is being retrieved from the outback or transferred, the flight nurse is typically the only one on the scene, or the doctor. So the use of AI in the outback will bring more equitable healthcare to patients.”
With more than 100,000 pre-loaded similar episodes of care loaded into the RFDS’ servers, clinicians can add their situational data to the app and be presented with care guidance based on previous outcomes.
“We’re using data not to dictate, but to complement the clinician. We like to call it extra pair of digital hands,” he says.
Look back on the week that was with hand-picked articles from Australia and around the world. Sign up to the Forbes Australia newsletter here or become a member here.